Abstract
Background
MGUS is a condition characterized by the presence of a monoclonal gammopathy without the clinical defining events of MM. All MM cases are preceded by MGUS, which is being diagnosed more frequently with use of more testing. In spite of major advances, our understanding of the pathogenesis of MGUS and MM remains incomplete. It is believed that the risk of MGUS transformation to MM is approximately 1% per year. Agent orange exposure has been linked to development of MM. We evaluated the risk of transformation of MGUS to MM and exposure to AO.
Methods
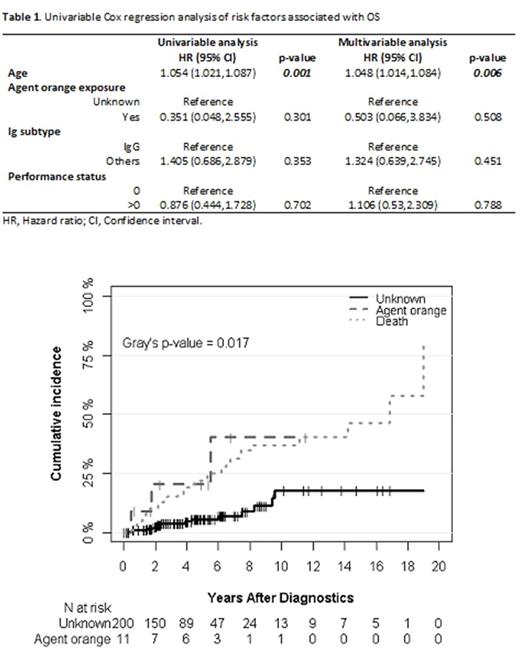
We performed a retrospective chart review of patients (pts) with MGUS who were seen at John D. Dingell Veterans Affairs Medical Center, Detroit MI between 1/2005-1/2015. We used disease codes: ICD9: 203.0 (multiple myeloma), 273.1 (monoclonal paraproteinemia) as well as ICD10: C90.0 (multiple myeloma), D47.2 (monoclonal gammopathy) to capture data. Data was collected on demographics, AO exposure, Ig subtype, comorbidities, and transformation to multiple myeloma. In a given pt, the date when M protein was first detected was considered as the date of MGUS diagnosis. Overall survival (OS) was calculated as the time from the date of MGUS diagnosis to death from any cause. Competing risk models were used to describe the distribution of the cumulative incidence rate of multiple myeloma by considering death as a competing risk. Univariable and multivariable subdistribution and Cox regression models were fit to assess associations of multiple myeloma and OS with the prechosen predictors (age, agent orange exposure, Ig subtype, and performance status).
Results
Total of 372 pts were identified using the above mentioned ICD codes. 141 pts were excluded from this analysis as 112 had MM, 10 had plasmacytoma, 10 had light chain disease and 9 had smoldering myeloma at the time of their initial presentation. 20 pts were ineligible as they were coded inaccurately. 211 pts with MGUS were identified; median age was 66 yrs (44-91). 96% (203) were male and 58% (122) were African Americans. 63% had an IgG type. 11 pts had reported AO exposure. Most pts had good PS (ECOG PS of 0-1). 17 pts had progressed to MM over a median follow up time of 17 years. Cumulative incidence rate (CIR) was 1.4% at 1 yr in all pts. In the AO exposure group, the CIR was 9.1% at 1 yr and 40.3 % at 10 yrs, while these were 1.0% at 1 yr and 19% at 10 yr in the non-exposed group. AO exposure was associated with higher risk of transformation to MM on univariable analysis (HR, 4.45; 95% CI,1.19 to16.67; p=0.027) and on multivariable analysis (HR, 11.19; 95% CI, 2.10 to 59.47; p=0.005). However, AO exposure was not associated with OS on multivariable analysis (HR, 0.50; 95% CI, 0.07 to 3.83; p=0.508)
Conclusion
In this single center study, we demonstrated that progression from MGUS to MM in our institution is similar to known literature at 1 %. AO exposure in our patient population lead to an increase in CIR, suggesting possible changes in disease biology and genetics. More in-depth studies and genetic analyses are warranted to further investigate the association of AO exposure to MM progression in MGUS pts.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal